Addressing Male Health Problems in Australia – with Dr Adam Ellerby
BY TRACEY HORDERN
There is plenty of research that suggests women live longer than men, and that most women enjoy better health over their lifetime than their male counterparts*.
This distortion of health is evident across all age groups.
But why is this the case? There are several working theories that try to explain why women enjoy better health outcomes than men – and these often boil down to societal and psychological reasons.
In practical terms, more women seek out medical help, resulting in more money being spent on the healthcare needs of women. Research shows that men visit their doctor less than women and consequently, are more likely to have a serious condition revealed when they do eventually attend.
But this is only part of the bigger picture.**
Men at Work
There are more men than women in full-time employment in Australia. This can impede on men seeking out a medical appointment in a timely fashion. Men also tend to work in more physically demanding jobs, with this type of employment often being more high-risk work, such as construction and mining.
Research also shows that there is a direct link between male employment and men’s health. Even today, many men feel that it is their duty to be the ‘bread-winners’. Male self-esteem is also often closely linked to their employment status. An unemployed man is more likely to feel a negative impact of their work status on their self-esteem and their mental health, compared to women.**
The ‘Macho’ Effect on Men’s Health
While the reasons men across all age groups seem to be not as healthy as women can be partly biological, the approach to addressing their health needs also plays a role.
Western societies have historically promoted the image of the strong, silent type as the ideal male identity. This can lead to men sometimes minimising and even ignoring a health concern. This in turn can lead to procrastinating seeking medical help, which can then allow a health concern to become more serious than if they were to seek out an appointment, sooner rather than later.
Men also often prefer to see a male doctor, especially if they perceive their health concern to be of a sensitive nature. If a male doctor is not available, this can also lead to even more of a barrier. Men can also have an unhelpful attitude that it is ‘weak’, to admit they are feeling unwell. This is even more prevalent if the condition of concern is a mental health issue.

Men’s Health and Mental Health Matters
Poor mental health can also manifest in men engaging in unhelpful coping mechanisms, such as self-medicating with alcohol and/ or drugs. This negative, self-medicating behaviour can compound, causing other related health consequences. Other health issues can also present as a result of poor mental health, such as cardiovascular disease and diabetes.***
Top 10 Causes of Death in Australian Men
According to data collected by the Australian Bureau of Statistics in 2016, the leading causes of death for Australian men include, in order from first to last:
- Heart disease
- Trachea and lung cancer
- Dementia and Alzheimer’s disease
- Cerebrovascular diseases
- Chronic lower respiratory diseases
- Prostate cancer
- Colon and rectum cancer
- Diabetes
- Blood and lymph cancer, including leukaemia
- Suicide
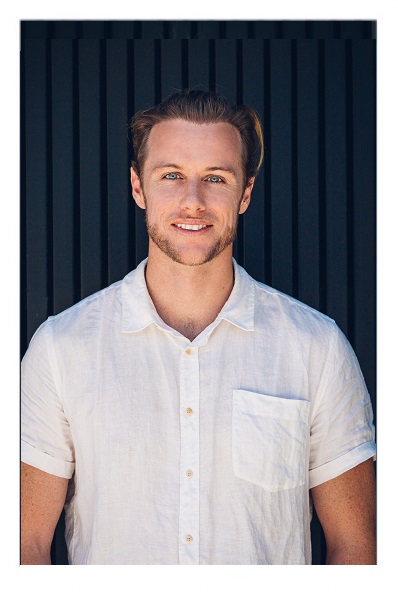
Improving Men’s Health Outcomes with Dr Adam Ellerby, GP
First Light Health’s Dr Adam Ellerby is General Practitioner, who is passionate about preventive and general health, with a special interest in sport and exercise medicine. As a male GP, Dr Adam Ellerby treats a large number of men and over the years, he has definitely seen and collated a pattern pattern that backs the national research findings.
The top things Dr Adam Ellerby see with men’s health (not in any particular order) include:
- Cardio-vascular disease –
“Usually there are no symptoms until it is too late. Health checks are a great way to pick things up early with screening”. - Sexual health and dysfunction –
“Although things are progressing, this is still an intimate and somewhat taboo area. The thing I tell everyone is “it’s all very common and nothing to be ashamed about”. - Mental health / suicide –
“Men traditionally present in subtle ways when they’re struggling. They tend not to cry or feel necessarily down. Often, they may present angrier or more withdrawn. With 70 plus per cent of suicides occurring in middle aged men, this is an area that’s often missed.” - Drug and alcohol misuse –
“This can often be coping strategies for both men and women. I want men to feel more supported and rely on healthier support mechanisms. We should be talking about our health and talking about when we’re struggling”. - Skin checks /skin cancer –
“Regular skin checks are recommended and can detect skin cancers at earlier, more treatable stages. It’s a great chance to chat about UV protection and other healthy lifestyle habits.”
Dr Ellerby has also witnessed a proportion of his male patients not prioritising their health, resulting in less than optimal outcomes. “A lot of it boils down to lack of engagement,” explains Dr Ellerby. “And often this is due to social expectations like stoicism/machismo, or due to lack of health literacy.”
“Men tend not to present with your ‘stereotypical’ mental health issues of appearing sad or crying more. Instead they may be more short-tempered or disengaged compared to normal. This leads to a more difficulty recognising there is a problem.”
“My current targets are to engage younger men in preventative health care – and to help build a culture that seeking help is normalised and not a sign of failure or weakness. I want men to talk about their health and talk about when they’re struggling”
– Dr Adam Ellerby
“So far, I get really good results by capturing guys in a ‘health check’ scenario where they may have only presented for something minor like an injury. Building a rapport is really important. It’s amazing how positive it can be. A lot of guys may have never had anyone to care about their health – including themselves!”
Where to Get Help
- Your GP (doctor)
- Lifeline – 13 11 14
- Suicide Call Back Service – 1300 659 467
- MensLine Australia – 1300 78 99 78
- Australian Men’s Shed Association Tel. 1300 550 009
Resources:
*Centre for Healthy Brain Ageing (CHeBA), UNSW Sydney
https://cheba.unsw.edu.au/blog/why-do-women-live-longer-men
**Health Direct Australia
https://www.healthdirect.gov.au/blog/the-health-problems-facing-australian-men-today
***Better Health Australia
https://www.betterhealth.vic.gov.au/


